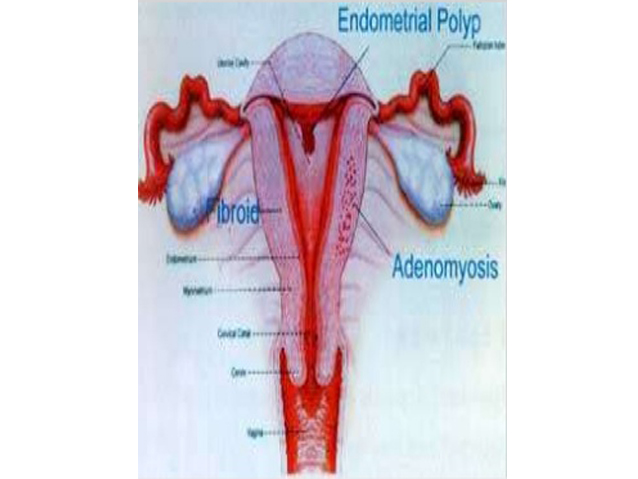
Pregnancy is a common cause. Polyps or fibroid (small and large growths) in the uterus can also cause bleeding. Rarely, a thyroid problem, infection of the cervix, or cancer of the uterus can cause abnormal uterine bleeding. In most women, abnormal uterine bleeding is caused by a hormone imbalance.
Abnormal uterine bleeding is bleeding from the vagina that occurs frequently or irregularly or lasts longer or is heavier than normal menstrual periods. The most common type of abnormal bleeding results from changes in the hormonal control of menstruation. This type is called abnormal uterine bleeding due to ovulatory dysfunction (AUB-O).
- Abnormal uterine bleeding is diagnosed when the physical examination, ultrasonography, and other tests have ruled out the usual causes of vaginal bleeding.
- An endometrial biopsy is usually done.
- The bleeding can usually be controlled with estrogen plus a progestin (a synthetic female hormone) or progesterone (similar to the hormone the body makes) or sometimes with one of these hormones alone.
- If the biopsy detects abnormal cells, treatment involves high doses of a progestin and sometimes removal of the uterus.
In about 90% of cases, the ovaries do not regularly release an egg (ovulate). Thus, pregnancy is less likely. However, because the ovaries may occasionally release an egg, these women should use contraception if they do not wish to become pregnant.
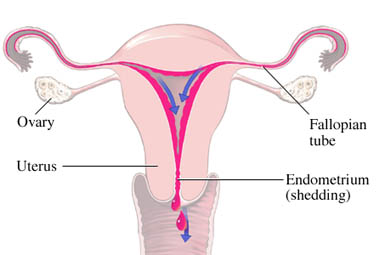
Abnormal uterine bleeding commonly results when the level of estrogen remains high instead of decreasing as it normally does after an egg is released and is not fertilized. The high estrogen level is not balanced by an appropriate level of progesterone. In such cases, no egg is released, and the lining of the uterus (endometrium) may continue to thicken (instead of breaking down and being shed normally as a menstrual period). This abnormal thickening is called endometrial hyperplasia. Periodically, the thickened lining is shed incompletely and irregularly, causing bleeding. Bleeding is irregular, prolonged, and sometimes heav
Symptoms
Bleeding may differ from typical menstrual periods in the following ways:
- Occur more frequently (fewer than 21 days apart—polymenorrhea)
- Occur frequently and irregularly between periods (metrorrhagia)
- Involve more blood loss (loss of more than about 3 ounces of blood or periods that last more than 7 days) but occur at regular intervals (menorrhagia)
- Involve more blood loss and occur frequently and irregularly between menses (menometrorrhagia)
Bleeding during regular menstrual cycles may be abnormal, or bleeding may occur at unpredictable times. Some women have symptoms associated with menstrual periods, such as breast tenderness, cramping, and bloating, but many do not. If bleeding continues, women may develop iron deficiency and sometimes anemia. Whether infertility develops depends on the cause of the bleeding.
Diagnosis
To exclude other possible causes, they ask about other symptoms and possible causes (such as use of drugs, the presence of other disorders, fibroids, and complications during pregnancies).A physical examination is also done. A complete blood count can help doctors estimate how much blood has been lost and whether anemia is present. A pregnancy test is also done.Tests to check for possible causes of vaginal bleeding may be done based on the findings during the interview and physical examination. For example, doctors may do blood tests to determine how fast blood clots (to check for clotting disorders).Doctors typically do blood tests to measure hormone levels (to check for polycystic ovary syndrome, thyroid disorders, pituitary disorders, or other disorders that are common causes of abnormal bleeding). Hormones that may be measured include female hormones such as estrogen or progesterone (which helps control the menstrual cycle), thyroid hormones, and prolactin.If results of these tests are negative, abnormal uterine bleeding is diagnosed.
Other tests
Transvaginal ultrasonography (using a small handheld device inserted through the vagina to view the interior of the uterus) is often used to check for growths in the uterus and to determine whether the uterine lining is thickened. Thickening of the uterine lining may result from noncancerous conditions such as polyps or fibroids or hormonal changes. (The hormonal changes that cause abnormal uterine bleeding can result in such thickening, which may cause precancerous cells to develop and increase the risk of endometrial cancer.)Transvaginal ultrasonography is done if women have any of the following (which includes most women with abnormal uterine bleeding):
- Age 35 or older
- Risk factors for endometrial cancer, such as obesity, diabetes, high blood pressure, polycystic ovary syndrome, and excess body hair (hirsutism), regardless of age
- Bleeding that continues despite treatment with hormones
- Pelvic or reproductive organs that cannot be examined adequately during the physical examination
- Findings suggesting abnormalities in the ovaries or uterus based on the physical examination
Transvaginal ultrasonography can detect most polyps, fibroids, endometrial cancer, and areas of thickening in the lining of the uterus (which may be precancerous). If transvaginal ultrasonography detects areas of thickening, other tests may be done to check for small polyps or other masses. One or both of the following tests may Hysteroscopy is done in the doctor’s office. If the doctor’s office cannot provide hysteroscopy, the procedure can be done in a hospital as an outpatient procedure.
An endometrial biopsy is usually also done to check for precancerous changes and for cancer in women with any of the following:
- Age 35 or older plus one or more risk factors for endometrial cancer (see above)
- Age under 35 plus several risk factors for endometrial cancer
- Bleeding that is persistent, irregular, or heavy despite treatment
- Thickening of the uterine lining (detected by transvaginal ultrasonography)
- Inconclusive findings during transvaginal ultrasonography
Treatment
- A drug to control the bleeding
- If bleeding continues, a procedure to control the bleeding
- If abnormal cells are present, high doses of a progestin or progesterone or, in postmenopausal women, sometimes removal of the uterus
Treatment of abnormal uterine bleeding depends on
- How old the woman is
- How heavy the bleeding is
- Whether the uterine lining is thickened
- Whether the woman wishes to become pregnant
Treatment focuses on controlling the bleeding and, if needed, preventing endometrial cancer.
Other treatments
If the uterine lining remains thickened or the bleeding persists despite treatment with hormones, hysteroscopy is usually done in an operating room to look into the uterus and is followed by dilation and curettage (D and C). For a D and C, tissue from the uterine lining is removed by scraping. This procedure may reduce bleeding. However, in some women, it causes scarring of the endometrium (Asherman syndrome), which can cause menstrual bleeding to stop (amenorrhea).If bleeding continues after a D and C, a procedure that destroys or removes the lining of the uterus (endometrial ablation) can often help control bleeding. This procedure may use burning, freezing, or other techniques.Endometrial Ablation
If bleeding continues to be substantial after other treatments have been tried, doctors may recommend removal of the uterus (hysterectomy).If the uterine lining contains abnormal cells (particularly in women who are older than 35 and who do not want to become pregnant), treatment begins with a high dose of a progestin. A biopsy is done after 3 to 6 months of treatment. If it detects abnormal cells, a hysterectomy is done because the abnormal cells may become cancerous. If women are postmenopausal, treatment does not begin with a progestin unless they have a condition that makes surgery risky. Hysterectomy may be required.
Emergency treatment
Rarely, very heavy bleeding requires emergency measures. They may include fluids given intravenously and blood transfusions.
Occasionally, doctors insert a catheter with a deflated balloon at its tip through the vagina and into the uterus. The balloon is inflated to put pressure on the bleeding vessels and thus stop the bleeding.
FAQ about AUB
Sometime patients have some questions and myths in their mind so we tries to answer some of them below.